Blepharitis



(Roll the mouse over blepharitis subtypes to view photos and descriptions)
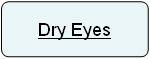
Blepharitis refers to chronic inflammation of the eyelids. Blepharitis is one of the most common disorder of the eye and is often the underlying reason for eye discomfort, redness and tearing. Other eye symptoms of blepharitis include: Burning, itching, light sensitivity, and an irritating, sandy, gritty sensation that is worse upon awakening.
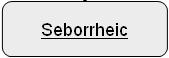
There are 3 forms of blepharitis (staphylococcal, seborrheic and MGD). All three forms of blepharitis are chronic in nature. Patients with staphylococcal blepharitis are relatively young (mean age 42 years) with a short history of ocular symptoms (mean 1.8 years). Patients with seborrheic blepharitis and MGD blepharitis are generally older and have a longer history of ocular symptoms.
In staphylococcal blepharitis there is scaling and crusting along the eye lashes. In seborrheic blepharitis there is greasy scaling along the eyelashes. Patients frequently have seborrheic dermatitis as well. In Meibomian gland dysfunction (MGD) there are prominent blood vessels crossing the eyelid margin. In addition there is pouting or plugging of meibomian gland openings, and poor expressibility and/or turbidity of the oily meibomian secretions. Patients with MGD frequently are noted to have coexisting rosacea and seborrheic dermatitis (Rosacea's Red Face). Use of isotretinoin (Accutane), an oral medication for severe cystic acne, has also been implicated as a cause of blepharitis.
Blepharitis Treatment
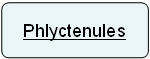
Blepharitis is a chronic disease for which there is no cure, and requires long-term treatment to keep it under control. Treatment consists of 2 phases (Acute phase and Maintenance phase). Acute phase treatment involves intensive therapy to rapidly bring the disease under control. In the maintenance phase the goal is to indefinitely continue the minimum amount of therapy that is necessary to keep the disease quiet. Herein we will not focus on the treatment of specific steroid responsive complications of blepharitis like marginal ulcers and phlyctenules, as they are less common and require specific diagnosis. We will focus on the treatments that help control the blepharitis process itself. Needless to say, controlling blepharitis itself, will reduce all the other blepharitis related complications.
Warm Compresses followed by Lid Scrubs is the most critical element of effective blepharitis control. This therapy removes the eyelid debris (which can be colonized by bacteria), reduces the bacterial load (mechanically as well as by lysis of bacteria due to detergent action of the soap in lid scrubbing) and stabilizes the tear film by releasing oily secretions from the meibomian glands, thus reducing tear evaporation (so the dry eye symptoms are also reduced).
Warm Compresses
Warm compresses heat the debris and crust on the lid margin to or above the melting point of their individual components so that they are easily removed with the lid scrubs.
Technique: Soaking a washcloth in water as warm as the eyelids can stand, and then placing the cloth on the lid surface (eyelids closed) for a five to ten minute period. In the acute phase this is performed 2 to 4 times day.
We have read about variations/innovations in the way warmth may be applied to the eye. One method described is the use of a fresh-boiled egg (in its shell wrapped in a washcloth). Another method described is to use a stocking filled with grains of uncooked dry rice heated in a microwave oven to a comfortable warm temperature.
Warm compresses may be combined with eyelid massage. This is especially important in patients who have Meibomian gland dysfunction (MGD). An analogy here will clarify the issue. In MGD the meibomian secretions are turbid and the gland openings are clogged. Think of a toothpaste tube which has butter (instead of toothpaste). When cold, you will not be able to express the butter out of the tube. However, once you heat it, then the butter will soften enough to come out of the tube, but pressure on the tube (squeezing) would still be necessary. Going by this analogy, after warm compresses, the turbid meibomian gland secretions are more fluid, but massage is necessary to express them. Therefore after every 1 minute of warm compresses, massaging the eyelid as follows will be useful:

Gently close the eyelids. Put your index finger on the outer corner of the eyelid. Pull the eyelid towards the ear, so that the eyelids are stretched taut. Next use the index finger of the opposite hand to apply direct pressure to the taut eyelids starting at the inner aspect of the eyelid near the base of the nose. Sweep with firm but gentle pressure towards the ear. Repeat this maneuver four to five times. Remember that the goal is to apply gentle pressure to the eyelids - so just rubbing the eyelid surface will do you no good (Ophthalmol Clin N Am 2003;16:37-42).
Lid Scrubs
There are several ways of performing lid scrubbing. You can choose whichever one you are most comfortable with. The scrubbing should be directed at the base of the eyelashes on the eyelid margin. Soaps (cleansing agent used) should not have excessive perfume or lotion content.
Neutrogena bar soap: This bar soap is used to form lather on the clean finger tips. Lather is then applied with fingertips on the eyelid margin and eyelash bases for up to 1 minute (with eyelids gently closed so that soap does not enter the eye). This is followed by a facial rinse.
Johnson's Baby Shampoo: The baby shampoo is first diluted one-to-one with water in a 'cup' in the palm of the hand. This is then mixed by rubbing with the clean fingertips and then applied in a gentle oval scrubbing motion to the margin and eyelash bases of the closed eyelid for 1 minute, followed by a fresh water facial rinse.
The soap solution (bar soap or baby shampoo) can alternatively be diluted in a container (e.g. plastic cup) and scrubbing performed using a washcloth wrapped around a finger (after dipping it in the diluted soap solution. A cotton tip applicator may be used alternatively.

There are commercially available cleansing pads that are presoaked in a cleansing solution (OCuSOFT Lid Scrubs or Novartis Eye-Scrub). These cleansing pads are equally effective albeit more expensive method of lid scrubbing and are claimed to be less irritating to the eyelids. One study showed then to be preferred choice by patients as compared to other methods of lid scrubbing (CLAO Journal 1996;22:209-12).
Antibiotic treatment
The use of an ointment on the eyelid margin immediately after lid scrubbing may help to increase patient comfort. The choice here is usually Erythromycin eye ointment or Tobradex eye ointment (steroid-antibiotic combination). In addition, the antibiotics help to further reduce the bacterial load on the eyelids.
Oral tetracyclines (doxycycline or minocycline) for about 3 months can be used in recalcitrant Meibomian Gland Dysfunction (MGD) cases. Tetracycline antibiotics affect the meibomian gland secretions, inhibit bacterial lipases as well as reduce the eyelid bacterial load.
Anti-Inflammatory treatment
Castor oil has been used traditionally in folk medicine as an anti-inflammatory remedy for treatment of blepharitis. The main ingredient in Castor oil is ricinoleic acid. Castor oil could either increase or decrease eyelid inflammation depending upon whether it is used only once or is used several times for many days. Eyelid inflammation may increase initially after starting treatment but with repeated use over a week, the blepharitis inflammation will be reduced. (Naunyn Schmiedebergs Arch Pharmacol 2001;364:87-95). Refresh Endura tears is a Castor oil emulsion. Restasis eyedrops has Castor oil in addition to cyclosporine.
As already discussed under 'Oral Treatment' of Dry Eyes, increasing the intake of Omega-3 fatty acids (flaxseed oil supplements) may also reduce the blepharitis inflammation.
Read more about Managing Blepharitis.
Antioxidant treatment
Eating more grapes may help blepharitis patients. The formation of oxidants like nitric oxide in the involved eyelid margin have been speculated to play a role in blepharitis (Cornea 2000;19:654-58). The substance, known as resveratrol is an anti-oxidant that is very effective against these nitrite type of oxidants. Grapes are particularly good sources of resveratrol. Resveratrol is found in the skin (not flesh) of grapes. Fresh grape skin contains about 50 to 100 micrograms of resveratrol per gram and red wine (also rich in resveratrol) contains about 1.5 to 3 milligrams per liter.
N-acetylcysteine (NAC), is an amino acid that enhances the production of glutathione, one of the body's most powerful antioxidant enzymes. In one reported study the effect of 100 mg of N-acetylcysteine orally, three times each day for 8 weeks. This treatment resulted in stabilization of tear film and reduced discomfort of blepharitis (Cornea 2002;21:164-8). Oral N-acetylcysteine treatment for blepharitis needs further evaluation. N-acetylcysteine is a 'supplement', therefore is available over the counter or in health food stores without prescription. We came across several NAC brands (Twinlabs, Solgar, Now Foods, Puritan's Pride). It is essential that you consult your doctor prior to initiating any treatment.
Cosmetic (Eye Makeup) use and Eyelid Dermatitis (a commonly missed association)
Contact allergic dermatitis could be caused by many products used for eye makeup. Mascara, eye shadows, eyeliners, eyebrow pencils - all have ingredients to which you could be allergic. One could be allergic to makeup applicators and brushes. It is possible to be allergic to eye drops that you may be using or to the commercially available make-up removers and lid scrubs. Even ingredients used in nail enhancements / make-up (overlay, sculptures etc) can cause eyelid dermatitis when you touch the eyes. You could be allergic to nickel found in house keys or car keys. When you touch the eyes, it can transfer to eyelids and cause dermatitis.
Contact allergic dermatitis of the eyelid will present as eyelid puffiness and parchment-like wrinkling of skin. Itching and redness in the involved area is possible. Allergic eyelid dermatitis may be mistaken for blepharitis. The treatment here is removing contact with the allergen, therefore blepharitis treatment will not work. Since there are so many ingredients inside the cosmetics to which you could be allergic, we recommend discontinuing all eye and nail make-up, getting allergy testing and then to resume eye and nail make-up, one at a time. If the allergy testing reveals reaction to some ingredient, then you cannot use that make-up product. As a temporary measure, a steroid ointment like Tobradex may help to provide relief from symptoms. Long term steroid use on the delicate eyelid skin may result in skin atrophy, skin discoloration or skin telangiectatic vessels. In a recent report, Tacrolimus ointment 0.03% was used twice daily on eyelid skin of patients with atopic dermatitis with good results (Am J Ophthalmol. 2003;135:297-302). Since Tacrolimus is a non-steroidal macrolide immunomodulator, it does not cause steroid-related skin changes.
We recommend epicutaneous patch testing (allergy testing) using the T.R.U.E Test, cosmetic series, steroid series as well as personal cosmetic products. The T.R.U.E test is for 24 antigen only and may not be able to identify your allergic antigen. Therefore your personal cosmetic products are to be tested for allergy as well.
There are important issues with mascara containing kohl. Also called al-kahl, kajal or surma, this color additive has been linked to lead poisoning in children and is not approved for cosmetic use in the U.S. Applying surma by sharing the applicator is a major reason for the spread of Trachoma in developing countries. The FDA's Center for Food Safety and Applied Nutrition warns that kohl can be found in imported mascaras. Be sure to check the label: Sometimes "kohl" indicates the shade of a product, not the actual contents. Bacterial contamination of mascara is also common. We recommend replacing mascara every three months or sooner if it develops an unusual texture or odor.
We recommend reading the FDA article on Eye Cosmetic Safety, and the journal articles on this subject from this MedLine list.
This information site has been provided by varied UK and US eye doctors for patients with eye problems.
Once your eye doctor has made a diagnosis or recommended an investigation or treatment, then you will be able to find further explanation on this site.